Introduction
In the context of obesity and metabolic syndrome, this review will zero in on the essentials of Semaglutide treatment. This study lays the groundwork for Semaglutide’s potential use in treating a wide range of complex health problems by analyzing its mechanism of action, clinical efficacy, and safety profile. The next chapter examines the pros and cons of compounding pharmacies offering customized Semaglutide formulations. We will talk about the fundamentals of losing weight and managing metabolic syndrome with an emphasis on how including drugs like Semaglutide may help with long-term success. It also highlights the need for individualized treatment plans and the need for ongoing guidance and support from healthcare experts as people deal with the complexity of obesity and metabolic syndrome.
Methods
The collection and analysis of quantitative data is the primary quantitative approach in this study. To collect this information, we will utilize a survey questionnaire to collect data from a targeted population. The dataset will next undergo statistical analysis to reveal hidden relationships and patterns. Quantitative methods provide a comprehensive and rigorous examination of research problems by providing empirical data and numerical insights into the subject.
Discussion
Semaglutide in the Treatment of Obesity and Metabolic Syndrome
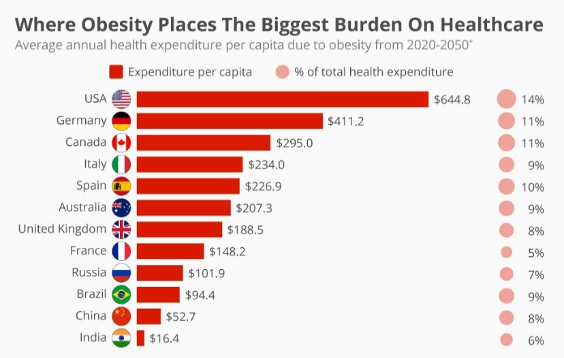
The use of Semaglutide for the treatment of obesity and metabolic syndrome has generated much discussion in the medical and scientific communities. Since obesity is still a significant international health concern with far-reaching repercussions, it is crucial to develop effective therapies, as shown in the infographic (Fig 1) below.

Figure 1. Obesity on a global scale. 21
Semaglutide is a GLP-1 receptor agonist that shows promise as a treatment option for obesity.1 Endogenous GLP-1 is a hormone that controls hunger and glucose metabolism, and this substance mimics its effects.2 Semaglutide is a multifunctional medicine whose effects extend beyond glycaemic control, incorporating cardiovascular protection and weight management advantages. This quality makes it applicable for treating both obesity and metabolic syndrome. Semaglutide works by stimulating GLP-1 receptors as the drug’s first effect. The beta cells of the pancreas and other organs have these receptors.1 By triggering insulin synthesis, they help keep blood sugar levels stable. GLP-1 receptor activation also increases feelings of fullness while decreasing appetite, making it easier to stick to calorie deficits and maintain a healthy weight.3 Because of its impact on both glucose metabolism and appetite management, Semaglutide helps treat obesity and metabolic syndrome. Clinical trials and studies have shown that Semaglutide may cause significant weight loss in those who are obese. Twenty-two patients have reported substantial reductions in body mass index (BMI), with average reductions above 10%.4 Improved metabolic indicators, such as lower blood glucose and glycated hemoglobin (A1c) levels, accompany weight reduction.22 Obesity arises from a complex interplay of factors that disrupt the balance of energy intake and expenditure (Figure 6). Various biological systems, genetic factors, and regulatory molecules maintain this balance and influence the susceptibility to obesity. Obesity develops and persists because of two related processes in the body. The first is the accumulation of fat tissue, which results from the interplay of genes, environment, and biology. The second is the body’s attempt to protect the excess fat tissue. This attempt gradually causes the fat tissue to malfunction. The impaired fat tissue then releases more inflammatory substances (such as TNFα and IL-6), makes less adiponectin, and does other things that cause inflammation and oxidative stress.23

Figure 2. Two-year effects of semaglutide in adults with overweight or obesity. 22
Semaglutide’s high clinical effectiveness in the treatment of metabolic syndrome makes it an essential tool for managing this illness. Semaglutide has shown excellent therapeutic efficacy and has a fantastic safety profile. The most frequent adverse effects are gastrointestinal disorders, including nausea and diarrhea, which are generally mild and manageable.2,3 Semaglutide is a good option for therapy because of its high therapeutic effectiveness and low safety risk.
Semaglutide, developed by Nordisk, developed different brand names: Ozempic, approved for type 2 diabetes, and Wegovy, which focuses explicitly on obesity management. These medications have a common origin but are approved for different diagnoses. The prescription varies as Wegovy is approved with a higher dosage to address obesity.
Despite its potential advantages, long-term monitoring of semaglutide’s safety and effectiveness in metabolic syndrome is essential. One of the vital parts of metabolic syndrome is obesity. Stoutness is characterized as the extreme collection of muscle versus fat, usually bringing about a weight file (BMI) of 30 or higher. A blend of hereditary, ecological, and social elements impacts an intricate condition. Weight essentially adds to the advancement of metabolic disorder, as an overabundance of fat tissue, especially in the stomach locale, prompts insulin obstruction, ongoing aggravation, and dysregulation of different metabolic cycles.3 The ongoing meaning of metabolic condition incorporates a few measures that should be met for determination. These models might change somewhat between various associations and rules; however, they, by and large, incorporate the presence of no less than three of the accompanying parts: abdominal obesity (estimated by abdomen circuit), high blood pressure, hypertriglyceridemia, diminished high-density lipoprotein (HDL) cholesterol levels, and high fasting glucose. Starting treatment for metabolic syndrome regularly centers around way-of-life adjustments to address the fundamental gamble factors. This incorporates dietary changes, expanded active work, and weight reduction. Weight reduction is essential in further developing insulin responsiveness. Due to the high incidence of multiple risk factors and comorbidities, it is crucial to understand how Semaglutide interacts with the different illnesses associated with metabolic syndrome.5 The impact on cardiovascular outcomes, medication interactions, and the implications of long-term Semaglutide treatment all require more study.1,4 When treating metabolic syndrome and weight gain, semaglutide is a game-changer. The fact that it works by modifying both glucose homeostasis and appetite control bolsters its credibility as a treatment option. There has to be additional study, especially in individuals with metabolic syndrome, to ensure its long-term effectiveness and safety despite its favorable safety profile. Because of its ability to enhance metabolic parameters, decrease weight, and boost overall well-being, semaglutide may aid in treating several complex and connected health issues.

Figure 3. Energy balance dysregulation of obesity.24
Compounding Pharmacies and Customised Semaglutide Formulations
Because of the challenges in obtaining some pharmaceuticals, such as Semaglutide, a GLP-1 receptor agonist used to treat obesity and metabolic syndrome, compounding pharmacies have gained prominence within the healthcare system.6 The replication of this medication poses ethical and legal concerns. Customized Semaglutide formulations from these specialty pharmacies are an essential alternative to the costly and inaccessible branded medications. The advantages and disadvantages of using compounding pharmacy are valid points of discussion. A regular compounding pharmacy may need more resources to ensure the high quality of such a compounded product. Compounding pharmacies specialize in making medicines that meet each patient’s unique needs.7 Due to the wide range of possible causes and effects of obesity and metabolic syndrome, tailoring treatment to each patient is essential. Compound Semaglutide formulations allow healthcare providers to tailor treatment plans to the unique needs of each patient who meets the requirements for weight loss medicine but needs access to the brand-name version due to cost or lack of insurance.8
One of the most critical steps in overcoming the difficulties connected with obesity is making Semaglutide available to individuals who need it. One strategy for tackling the worldwide pandemic of obesity is to make weight reduction drugs more widely available to those who qualify for them. Getting Semaglutide from compounding pharmacies is advantageous because of its customization options in terms of dosage, cost, and composition. Compounding pharmacies can accommodate the individualized dosing and administration demands of their patients. 6,7 This is particularly crucial Because of individual differences in reaction and the possibility of unwanted side effects. Those who cannot afford the name-brand version of Semaglutide have another choice in the shape of compounded Semaglutide formulations. By making care more widely available, we can tackle the public health problem of obesity from more angles.9 But weighing the benefits of compounding pharmacies against the hazards they may pose is critical. The primary emphasis centers on the regulation of compounded pharmaceuticals. Compound formulations are subject to less stringent regulatory examination than FDA-approved pharmaceutical medicines. The gap in regulatory supervision between the tailored Semaglutide and other versions of the medicine may give rise to apprehensions regarding its safety and efficacy. The potential for harm to patients and effects on treatment effectiveness arises from the compounded medications’ lack of standardization in quality and consistency.
More in-depth clinical evidence on the effects and safety of compounded Semaglutide formulations over the long term is also essential to remember. Clinical studies and other forms of stringent testing have generated a mountain of evidence favoring branded medicine.10 Patients and doctors may have less confidence in the long-term safety and effectiveness of compounded formulations because of a possible lack of data supporting them. The lack of openness and trustworthiness in compounded medicine procurement is another concern. Patients and doctors need to have trust in compounding pharmacies since the quality of the final product relies on their expertise and strict adherence to industry standards. Patients seeking tailored Semaglutide formulations to treat obesity and metabolic syndrome may, therefore, benefit from compounding pharmacies. More people will have access to treatment alternatives because of their flexibility and low cost10. However, the potential dangers of compounded pharmaceuticals regarding regulation, quality, and long-term safety and effectiveness must be considered alongside their advantages. Careful thinking and more study are necessary to guarantee that compounding pharmacies continue to play a significant role in tackling these complicated health challenges.
Weight Loss Strategies and Metabolic Syndrome Management
Dietary and lifestyle modifications and increased physical activity are often the cornerstones of treatment strategies for metabolic syndrome and weight reduction. For the complex health problems of obesity and metabolic syndrome11, these are essential components. In addition, combining these lifestyle adjustments with medications like Semaglutide has been discovered as a promising method for long-term treatment. There is a wide variety of changes one may make to their way of life that will positively impact their health and happiness. For those struggling with obesity and metabolic syndrome, these modifications might prove to be revolutionary. Adopting a balanced diet, participating in regular physical exercise, and addressing weight gain-causing habits are vital. In order to effectively treat metabolic syndrome, the patient must make long-term changes to their eating and exercise habits.13
Dietary adjustments help with both weight reduction and managing metabolic syndrome. Eating correctly may aid in shedding extra pounds, keeping you satisfied for longer, and controlling chronic conditions like insulin resistance.14 Eating more whole foods, fruits, vegetables, and lean meats while reducing consumption of processed and sugary meals might help you reach your target. It is crucial to tailor dietary recommendations to each patient based on their metabolic rate and food preferences.12,14 Semaglutide’s satiety-inducing and appetite-suppressing characteristics might help patients adopt healthy eating behaviors. Exercise is also essential in the treatment of metabolic syndrome and in the process of reducing weight. Heart health, insulin sensitivity, and caloric burn all benefit from regular exercise.15 Some exercise plans may need to change as they become more physically fit. Incorporating Semaglutide may enhance the effectiveness of physical exercise by lowering the burden of excessive hunger, promoting more activity, and assisting in sustaining weight reduction.
Combining pharmacological therapies like Semaglutide with lifestyle changes is a significant strategy for the effective and long-term management of medical disorders. Semaglutide’s appetite-suppressing and fullness-increasing mechanism of action is complementary to behavioral modification strategies.12 Semaglutide may be a complementary intervention for those who struggle to make and maintain dietary changes or to start engaging in regular physical activity. In addition to lowering body weight, Semaglutide improves metabolic markers, including blood glucose and A1c. These benefits may act as powerful incentives for people, underscoring the value of keeping up with lifestyle changes over the long term. Fourteen doctors should also oversee plans to combine dietary and supplement modifications with drug usage. Each patient has different needs and responses, so it is crucial to tailor treatment programs.15 Long-term success relies on careful monitoring and periodic adjustments to lifestyle and medication.
Modifying one’s diet and engaging in more physical activity are, thus, cornerstones of successful weight reduction and treatment of metabolic syndrome. Combining treatments like Semaglutide with these behavioral changes has the potential to provide long-lasting, beneficial effects on health. Medication therapy for obesity and metabolic syndrome is more likely to be successful and long-lasting when the medication’s mechanism of action is in sync with the goals of lifestyle modifications.15 The success of this integrated strategy relies heavily on the joint efforts of patients and healthcare providers.
Personalized Approaches to Obesity and Metabolic Syndrome Treatment
A paradigm shift has occurred toward individualized methods of treating obesity and metabolic syndrome, which take into account the individual needs and circumstances of each patient. These personalized methods emphasize the need to consider each patient’s unique traits and treatment responses to achieve optimal results in treating these complicated health issues.16. Patients need continuous assistance and direction from healthcare experts to help them reach and maintain a healthy weight. No one-size-fits-all approach exists for dealing with obesity and metabolic syndrome. Each individual’s sickness is a product of their genes. Their environment and their own choices and behaviors.17 As a consequence, success relies heavily on tailoring care to each patient’s individual needs. This tailored strategy extensively analyzes each patient’s medical history and lifestyle. With the results of this assessment in hand, doctors may create individualized plans of care to meet each patient’s needs best.18
Depending on the patient’s specific needs, customized treatment strategies include dietary advice and even medication like semaglutide. Customizing medication dosing and composition for each patient improves both safety and efficacy. 19 When providing individualized treatment, it is essential to address any mental health or behavioral issues that may either impede or facilitate development. In order to devise strategies that encourage adherence to the treatment plan. Obesity and metabolic syndrome are strict conditions to manage without the constant guidance of medical professionals.20 Maintaining long-term control of these conditions is often difficult to achieve. Professionals in the healthcare industry provide vital services beyond providing treatment16,18. Consistent follow-up with patients allows for assessment of recovery and troubleshooting.
Also crucial for long-term success is that medical experts may assist patients in setting reasonable objectives and expectations. Healthcare providers can help patients overcome challenges and stay on track as they strive to attain and maintain a healthy weight17. Additionally, healthcare practitioners may give consumers information and help, allowing them to make educated choices about their health and treatment options. It is impossible to emphasize the value of constant encouragement and direction from medical experts. The intricacy of obesity and metabolic syndrome demands thorough, long-term care19. Helping patients through recovery is only possible with the medical expertise, emotional support, and inspiration healthcare professionals provide. Thus, individualized approaches to treating obesity and metabolic syndrome20 consider each patient’s unique experiences and the need for specialized treatment. These strategies are crucial for improving therapeutic outcomes because they consider each patient’s individuality. Patients may achieve and maintain healthy weight results17,20 with healthcare professionals’ continued help and supervision. Patients and doctors must work together to overcome the many obstacles caused by various health conditions.
Conclusion
Using case studies, this chapter explains how Semaglutide helps people who are struggling with weight issues and metabolic syndrome. It sheds information on the medication’s mechanism of action, clinical effectiveness, and safety profile, pointing to its potential to improve patient outcomes. This chapter also highlights the value of compounding pharmacies in meeting patients’ needs for tailored Semaglutide formulations in a convenient and economical way. However, severe regulation and long-term safety reviews continue to be necessary. Furthermore, the study emphasizes the necessity of dietary changes, increased physical activity, and other lifestyle alterations as the fundamental factors of weight reduction and metabolic syndrome treatment. Combining Semaglutide with these behavioral modifications might be an effective strategy for achieving and sustaining better results. This chapter also underlines the need for tailored treatment plans that address each patient’s specific requirements and the need for continued medical support. This all-encompassing strategy aims to provide patients with the tools they need to navigate the challenging landscape of obesity and metabolic syndrome on the way to enhanced health and well-being.
References
- Alexopoulos SJ, Chen SY, Brandon AE, et al. Mitochondrial uncoupler BAM15 reverses diet-induced obesity and insulin resistance in mice. Nature Communications. 2020;11(1). doi: https://doi.org/10.1038/s41467-020-16298-2
- Ryan DH. Next-generation antiobesity medications: Setmelanotide, semaglutide, tripeptide, and bimagrumab: What do they mean for clinical practice? J Obes Metab Syndr. 2021;30(3):196-208. doi:10.7570/jomes21033
- Jung HN, Jung CH. The Upcoming Weekly Tides (Semaglutide vs. Tirzepatide) against Obesity: STEP or SURPASS? Journal of Obesity & Metabolic Syndrome. 2022;31(1):28-36. doi:https://doi.org/10.7570/jomes22012
- Li HL, Tsoi MF, Feng Q, et al., Prevalence of Childhood Obesity in the United States 1999 – 2018: A 20-Year Analysis. Journal of the Endocrine Society. 2021;5(Supplement_1):A24-A25. doi:https://doi.org/10.1210/jendso/bvab048.047
- Alexiadou K, Tan TM-M. Gastrointestinal Peptides as Therapeutic Targets to Mitigate Obesity and Metabolic Syndrome. Current Diabetes Reports. 2020;20(7). doi:https://doi.org/10.1007/s11892-020-01309-9
- Wojtara M, Syeda Y, Mozgala N, Mazumder A. Examining Off-Label Prescribing of Ozempic for Weight-Loss. Qeios Limited.com. They were published on June 6, 2023. https://www.researchgate.net/profile/Ashmita-Mazumder/publication/371339511_Examining_Off-Label_Prescribing_of_Ozempic_for_Weight-Loss/links/649c350ab9ed6874a5e3c766/Examining-Off-Label-Prescribing-of-Ozempic-for-Weight-Loss.pdf
- Tolentino J. Document – Gale Academic OneFile. go.gale.com. Published 2023. Accessed November 26, 2023. https://go.gale.com/ps/i.do?id=GALE%7CA749834342&sid=googleScholar&v=2.1&it=r&linkaccess=abs&issn=0028792X&p=AONE&sw=w&userGroupName=anon%7Eb93ec967&aty=open-web-entry
- Brayden DJ. The centenary of the discovery of insulin: an update on the quest for oral delivery. Frontiers in Drug Delivery. 2021 September 15;1:726675. https://go.gale.com/ps/i.do?id=GALE%7CA749834342&sid=googleScholar&v=2.1&it=r&linkaccess=abs&issn=0028792X&p=AONE&sw=w&userGroupName=anon%7E83378395&aty=open-web-entry
- Gleeson JP, Fein KC, Whitehead KA. Oral delivery of peptide therapeutics in infants: Challenges and opportunities. Advanced Drug Delivery Reviews. 2021 June 1;173:112-24. https://doi.org/10.1016/j.addr.2021.03.011
- Heffernan T. Obesity: Is the tide turning? http://www.rcsismj.com/wp-content/uploads/RCSIsmj_2023_Final.pdf
- Castro-Barquero S, Ruiz-León AM, Sierra-Pérez M, Estruch R, Casas R. Dietary strategies for metabolic syndrome: a comprehensive review. Nutrients. 2020 Sep 29;12(10):2983. https://doi.org/10.3390/nu12102983
- Wang HH, Lee DK, Liu M, Portincasa P, Wang DQ. Novel insights into the pathogenesis and management of the metabolic syndrome. Pediatric Gastroenterology, H& Nutrition. 2020 May;23(3):189. https://doi.org/10.5223%2Fpghn.2020.23.3.189
- Gheorghita Puscaselu R, Lobiuc A, Damian M, Covasa M. Alginate: from the food industry to biomedical applications and management of metabolic disorders. Polymers. 2020 Oct 20;12(10):2417. https://doi.org/10.3390/polym12102417
- Wang PX, Deng XR, Zhang CH, Yuan HJ. Gut microbiota and metabolic syndrome. Chinese Medical Journal. 2020 Apr 5;133(07):808-16. 1097/CM9.0000000000001553
- Jepsen S, Suvan J, Deschner J. The association of periodontal diseases with metabolic syndrome and obesity. Periodontology. 2000. 2020 Jun;83(1):125-53. https://doi.org/10.1111/prd.12326
- Mun S, Park K, Lee S. Evaluation of thermal sensitivity is of potential clinical utility for the predictive, preventive, and personalized approach advancing metabolic syndrome management. EPMA Journal. 2022 Mar;13(1):125-35. https://doi.org/10.1007/s13167-022-00273-6
- Sharpton SR, Schnabl B, Knight R, Loomba R. Current concepts, opportunities, and challenges of gut microbiome-based personalized medicine in nonalcoholic fatty liver disease. Cell Metabolism. 2021 Jan 5;33(1):21-32. https://doi.org/10.1016/j.cmet.2020.11.010
- Motevalli M, Drenowatz C, Tanous DR, Khan NA, Wirnitzer K. Managing childhood obesity—time to shift from generalized to personalized intervention strategies. Nutrients. 2021 Apr 6;13(4):1200. https://doi.org/10.3390/nu13041200
- Nilsson PM, Korduner J, Magnusson M. Metabolically healthy obesity (MHO)—new research directions for personalized medicine in cardiovascular prevention. Current Hypertension Reports. 2020 Feb; 22:1-5. https://doi.org/10.1007/s11906-020-1027-7
- Jayawardena R, Sooriyaarachchi P, Misra A. Abdominal obesity and metabolic syndrome in South Asians: prevention and management. Expert Review of Endocrinology & Metabolism. 2021 Nov 2;16(6):339-49. https://doi.org/10.1080/17446651.2021.1982381
- McCarthy N, and Felix R. “Infographic: Where Obesity Places The Biggest Burden On Healthcare.” Statista Daily Data, October 11, 2019, statista.com/chart/19621/annual-health-expenditure-per-capita-due-to-obesity/. It was accessed on November 8, 2023.
- Garvey WT, Batterham RL, Bhatta M, et al., Two-year effects of semaglutide in adults with overweight or obesity: the STEP 5 trial. Nature medicine. 2022 Oct;28(10):2083-91. https://doi.org/10.1038/s41591-022-02026-4
- Iacobini C, Pugliese G, Blasetti Fantauzzi C, Federici M, Menini S. Metabolically healthy versus metabolically unhealthy obesity. Metabolism. 2019;92:51-60. doi:10.1016/j.metabol.2018.11.009
- US Department of Health and Human Services. NIH Publication No. 98-4083. 1998